Common Eye Problems
Our eyes play a vital role in our daily lives, allowing us to perceive the world around us. However, various factors can impact our vision and eye health, leading to common eye problems. Understanding these common eye problems and their symptoms is crucial for seeking timely care and maintaining optimal eye health. Regular eye check-ups play a key role in detecting issues early, allowing for effective management, and preserving the gift of sight.
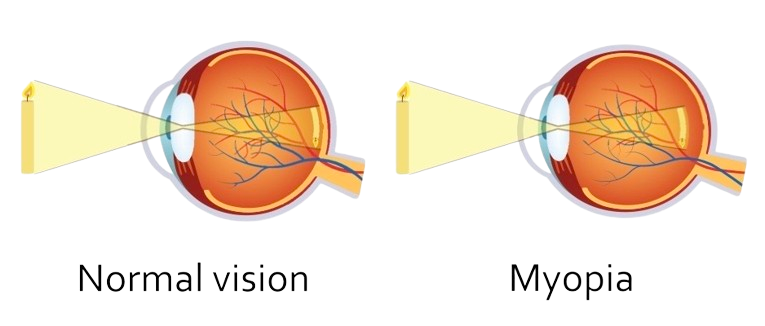
Myopia, commonly known as nearsightedness, is a refractive error of the eye where close objects are seen clearly but distant objects appear blurry. This occurs when the eyeball is too long or the cornea has too much curvature, causing light entering the eye to focus in front of the retina instead of directly on it.
1. Genetics: Myopia often runs in families, suggesting a strong genetic component.
2. Environmental Factors: Prolonged proximity to work, such as reading or computer use, can contribute.
3. Eye Strain: excessive strain on the eyes, especially during activities requiring close focus.
1. Blurred vision for distant objects.
2. Eye strain or discomfort.
3. Squinting to see clearly.
Low Myopia:
Diopter Range: Up to -3.00 D
Individuals with mild myopia may experience slight blurriness for distant objects but can usually see well without corrective lenses.
Moderate Myopia:
Diopter Range: Between -3.00 D and -6.00 D
Blurred vision for distant objects becomes more noticeable. Corrective lenses are usually prescribed.
High Myopia:
Diopter Range: Beyond -6.00 D
Severe blurriness for distant objects. There is a higher risk of associated eye conditions such as retinal detachment, glaucoma, and cataracts.
Apart from the severity classification, myopia can also be categorized based on its progression:
Simple Myopia:
Stabilizes in adulthood without significant progression.
Pathological Myopia:
Associated with structural changes in the eye, increasing the risk of complications. This includes a higher risk of retinal detachment, glaucoma, and macular degeneration.
It’s important to note that myopia can also be categorized by the age of onset:
Congenital Myopia:
Present at birth or develops in infancy.
Acquired Myopia:
Develops later in childhood or adolescence.
1. Prescription Glasses or Contact Lenses: Corrective lenses help focus light directly on the retina.
2. Refractive Surgery: Procedures like LASIK reshape the cornea for clearer vision.
3. Orthokeratology: the use of special contact lenses to reshape the cornea temporarily.