Retinal Diseases
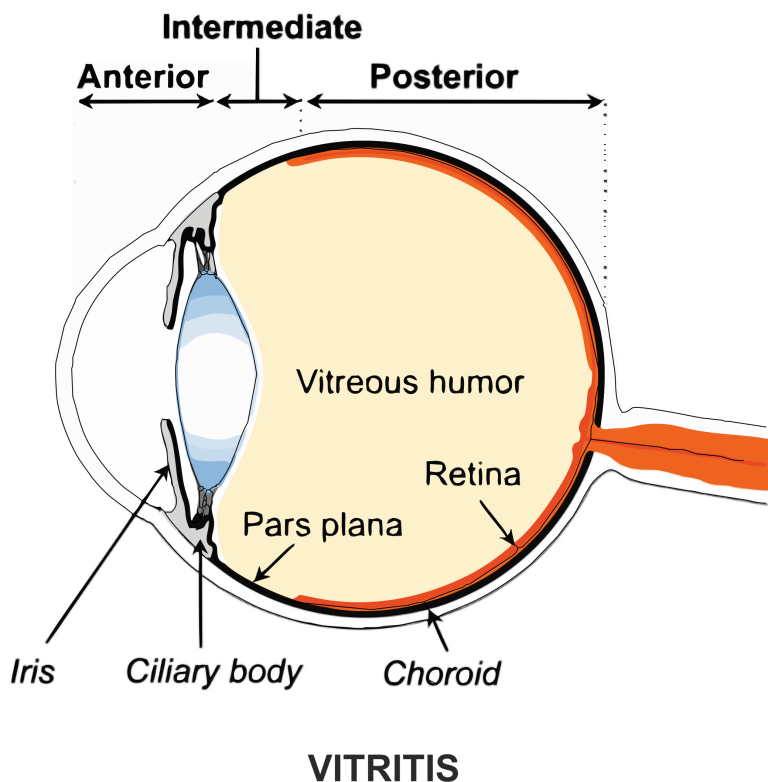
Retinal diseases affect the sensitive tissue at the back of the eye responsible for capturing light and sending signals to the brain.
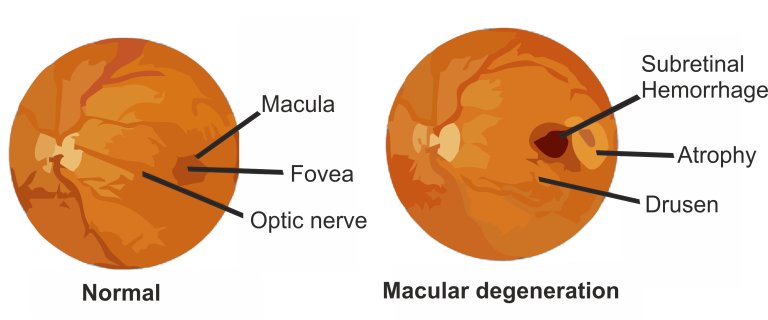
Age-Related Macular Degeneration (AMD) is a progressive eye disease affecting the macula, the central portion of the retina responsible for sharp, central vision. It is the leading cause of severe vision loss in people over 50.
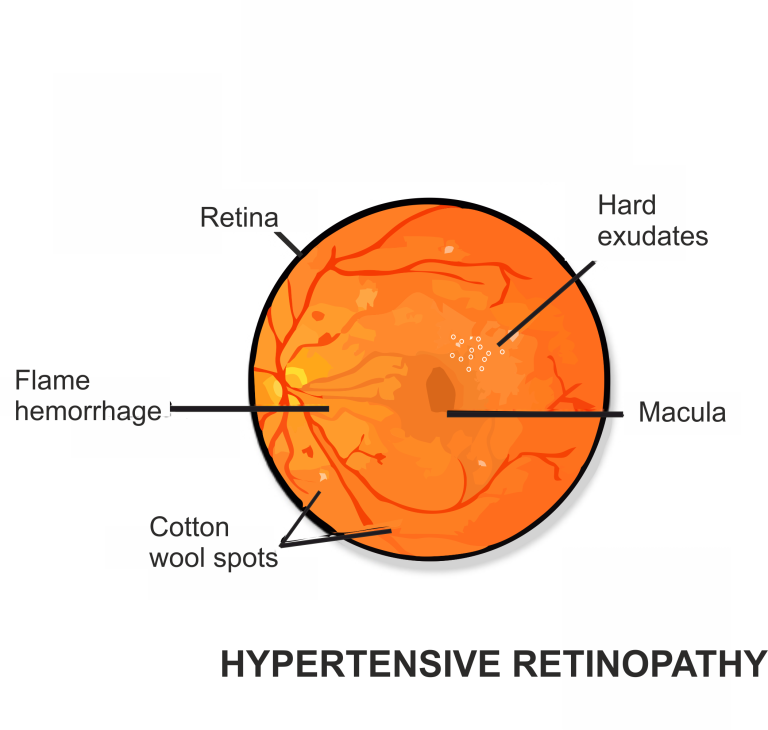
The primary cause of AMD is aging, particularly in individuals over 50. Other risk factors include a family history of AMD, smoking, hypertension, and certain genetic factors.
1. Blurred or distorted central vision.
2. Difficulty recognizing faces.
3. Straight lines appear wavy.
Dry AMD (Non-Neovascular): Characterized by the gradual breakdown of light-sensitive cells in the macula.
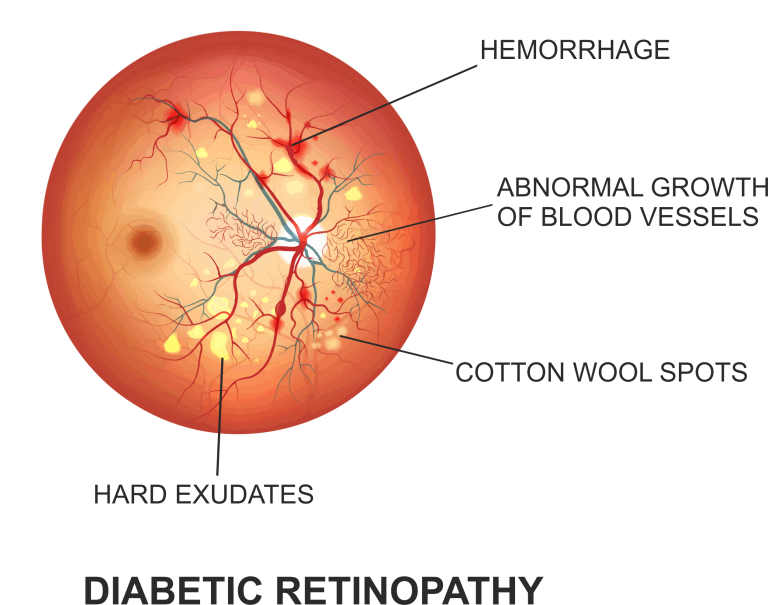
Wet AMD (Neovascular): Involves the growth of abnormal blood vessels beneath the retina, leading to leakage of blood and fluid.
Dilated Eye Exam: A comprehensive eye examination includes examining the retina for signs of AMD.
Amsler Grid Test: A grid with straight lines is used to detect any distortion in the central vision.
Optical Coherence Tomography (OCT): Produces detailed cross-sectional images of the retina.