vision for the future
Ramole Eye Hospital in Nashik is NABH Accredited Advanced Eye Care Centre in Nashik with all facilities like Advance PHACO Micro Surgery (MICS), Toric Lens Implant, New Refractive Tricofocal Implant, Contoura Lasik Vision Surgery, Advanced Surface Treatment, Phakic Implant (Phakic Lens/ICL), Keratoconus Treatment (C3R) etc. with Specialised & Customized Facilities available for All Age Groups including Pediatric to Senior Citizens. We provide all types of Mediclaim, ESIC, Facilities too.
GLAUCOMA SURGERY HELPS IN FOLLOWING EYE PROBLEMS

Diabetic Retinopathy
Diabetic retinopathy arises as a complication of diabetes, impacting the blood vessels located within the retina.
Retinal Vein Occlusion (RVO)
Retinal vein occlusion (RVO) occurs when one of the veins carrying blood away from the retina becomes blocked.
Glaucoma
Glaucoma encompasses a range of eye conditions marked by optic nerve damage, vital for relaying visual signals from the eye to the brain.
Selective Laser Trabeculoplasty (SLT) surgery
Selective Laser Trabeculoplasty (SLT) offers a less invasive approach to managing intraocular pressure in open-angle glaucoma. By targeting melanin-containing cells in the trabecular meshwork, SLT facilitates fluid drainage from the eye, reducing pressure without the risk of tissue damage associated with traditional laser treatments
Here’s an overview of the Selective Laser Trabeculoplasty (SLT) procedure:
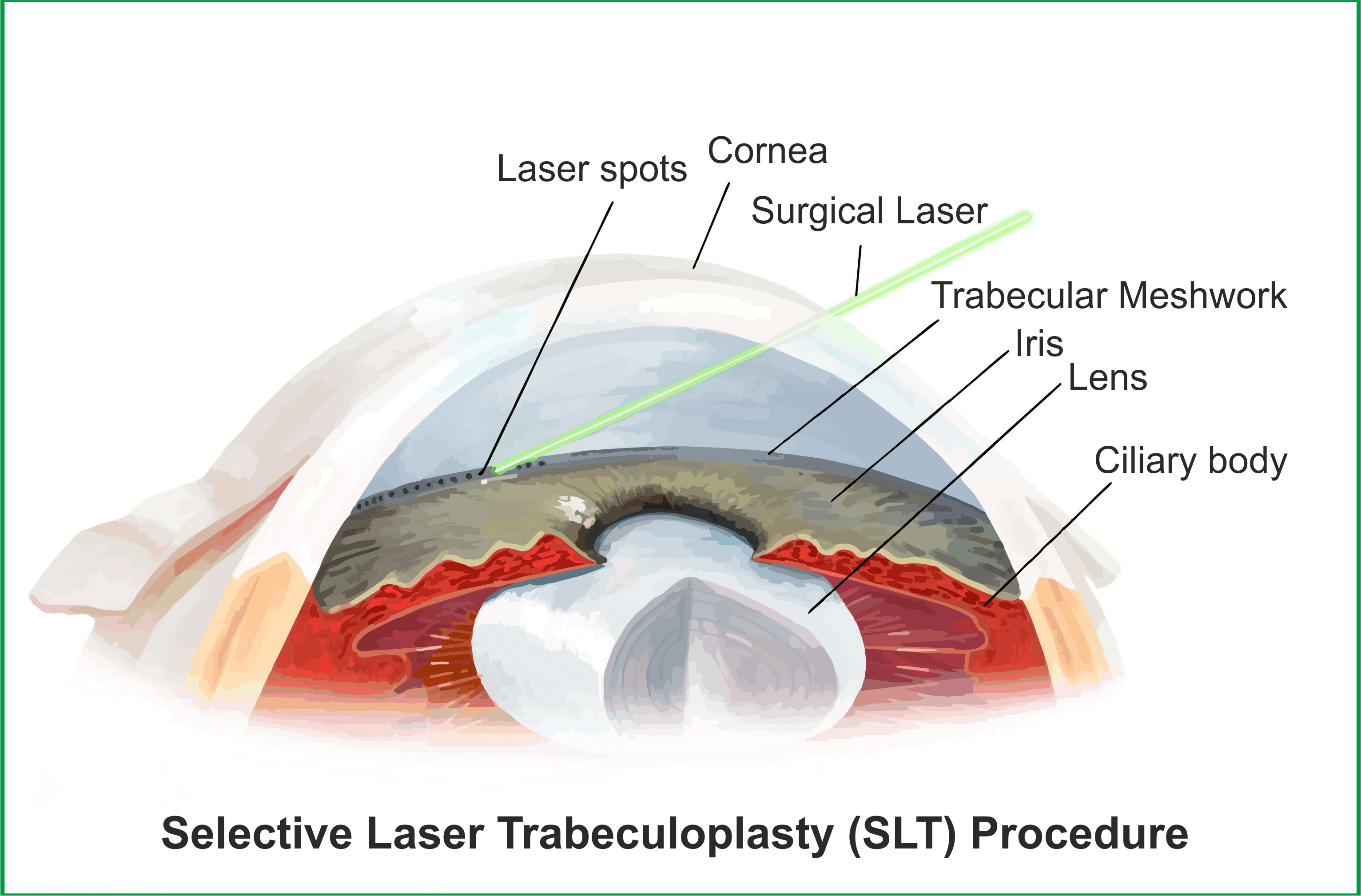
1) Preparation: The patient’s eye is numbed with eye drops to minimize discomfort during the procedure. The patient may also receive a mild sedative, if needed.
2) Positioning: The patient is positioned comfortably in a chair or on an examination table, with the affected eye held open by a speculum to keep it steady.
3) Targeting: Using a specialized laser system, the ophthalmologist precisely targets the trabecular meshwork, the drainage system within the eye, which regulates the flow of aqueous humor (the eye’s fluid).
4) Application: Short pulses of low-energy laser light are applied to the targeted area of the trabecular meshwork. The laser selectively targets melanin-containing cells, leaving surrounding tissue unharmed.
5) Treatment: The laser pulses stimulate a biological response in the trabecular meshwork, improving its ability to drain aqueous humor from the eye. This helps to reduce intraocular pressure (IOP) over time.
6) Completion: Once the treatment is completed, the ophthalmologist may administer additional eye drops to soothe the eye and prevent infection.
7) Post-procedure Care: The patient is usually able to resume normal activities immediately after the procedure. However, they may be advised to avoid strenuous activities or rubbing the eyes for a short period of time.
8) Follow-up: Patients typically return for follow-up appointments to monitor their intraocular pressure and assess the effectiveness of the SLT treatment. Additional SLT sessions may be recommended if needed.
Minimally Invasive Glaucoma Surgery (MIGS)
Minimally Invasive Glaucoma Surgery (MIGS) refers to a group of surgical procedures and devices designed to reduce intraocular pressure (IOP) in patients with glaucoma using minimally invasive techniques. Unlike traditional glaucoma surgeries, which are more invasive and carry higher risks of complications, MIGS procedures are typically performed through small incisions and aim to provide a safer and less traumatic option for managing glaucoma.
Here’s an overview of the Minimally Invasive Glaucoma Surgery (MIGS) procedure:
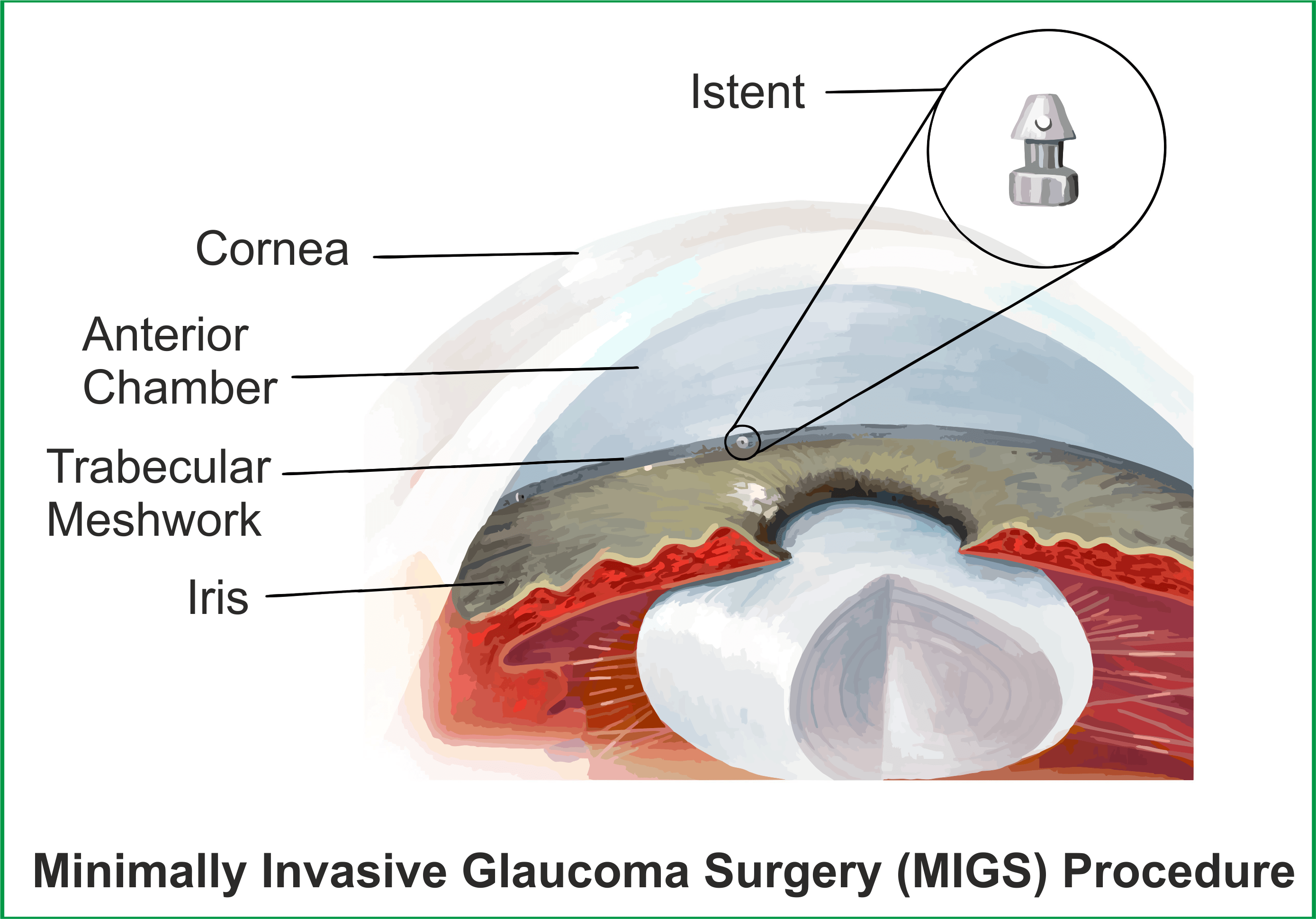
1) Preparation: The patient undergoes pre-operative assessments and evaluations to determine their suitability for MIGS surgery. This may include measurements of intraocular pressure (IOP), visual field tests, and imaging of the eye’s drainage structures.
2) Anesthesia: Before the procedure, the patient receives local anesthesia to numb the eye and surrounding tissues.
3) Access: A small incision is made in the eye to gain access to the anterior chamber, where the trabecular meshwork or other drainage structures are located.
4) Device Placement: The MIGS device, which could be a stent, shunt, or other microsurgical implant, is carefully inserted into the eye through the incision. The device is designed to improve aqueous humor outflow and reduce intraocular pressure.
5) Positioning: The surgeon positions the MIGS device in the appropriate location within the eye, ensuring optimal placement for effective drainage.
6) Securing the Device: Once positioned correctly, the MIGS device is secured in place to prevent movement or displacement.
7) Closure: The incision site is closed using sutures or a self-sealing technique, depending on the specific procedure and surgeon’s preference.
8) Post-operative Care: After the surgery, the patient receives instructions for post-operative care, which may include using antibiotic and anti-inflammatory eye drops, avoiding strenuous activities, and attending follow-up appointments.
9) Monitoring: Patients are monitored closely in the post-operative period to assess the effectiveness of the MIGS procedure in lowering intraocular pressure and managing glaucoma. Additional interventions or adjustments may be made as needed.
