vision for the future
Ramole Eye Hospital in Nashik is NABH Accredited Advanced Eye Care Centre in Nashik with all facilities like Advance PHACO Micro Surgery (MICS), Toric Lens Implant, New Refractive Tricofocal Implant, Contoura Lasik Vision Surgery, Advanced Surface Treatment, Phakic Implant (Phakic Lens/ICL), Keratoconus Treatment (C3R) etc. with Specialised & Customized Facilities available for All Age Groups including Pediatric to Senior Citizens. We provide all types of Mediclaim, ESIC, Facilities too.
CORNEA SURGERY HELPS IN FOLLOWING EYE PROBLEMS

keratoconus
Keratoconus is a progressive eye disorder causing corneal thinning and bulging, resulting in a cone-shaped cornea.
Cornea scarring
Corneal scarring is tissue damage or opacity on the cornea, caused by injury or inflammation, leading to reduced vision.
Fuchs' dystrophy
Fuchs’ dystrophy is an eye condition causing gradual corneal swelling, which leads to reduced vision.
Keratoconus C3R surgery
Keratoconus is a progressive eye disorder characterized by the thinning and bulging of the cornea, which results in a cone-like shape rather than the normal dome shape. C3R stands for Corneal Collagen Cross-Linking with Riboflavin, a treatment aimed at halting the progression of keratoconus and strengthening the cornea.
Here’s an overview of the Keratoconus C3R procedure:

1) Preparation: The patient’s eye is numbed with local anesthesia, and a speculum is used to keep the eyelids open.
2) Riboflavin Application: Riboflavin eye drops, which contain vitamin B2, are applied to the surface of the cornea. These drops help to enhance the cross-linking process.
3) Ultraviolet Light Exposure: After riboflavin application, the cornea is exposed to ultraviolet (UV) light for a specific duration. The UV light activates riboflavin, which induces the formation of bonds (cross-links) between collagen fibers in the cornea.
4) Cross-Linking Process: The cross-linking process strengthens the cornea by increasing its rigidity and stability. This helps to halt the progression of keratoconus and prevent further thinning and bulging of the cornea.
5) Post-operative Care: After the procedure, patients may experience some discomfort and light sensitivity. They are prescribed antibiotics and anti-inflammatory eye drops to prevent infection and reduce inflammation. Patients are advised to avoid rubbing their eyes and to follow their surgeon’s instructions for post-operative care.
Oculoplasty surgery
Oculoplasty is a specialized field of ophthalmology that focuses on the diagnosis and management of disorders related to the eyelids, orbit (eye socket), tear ducts, and surrounding facial structures.
Here’s an overview of the Oculoplasty procedure:
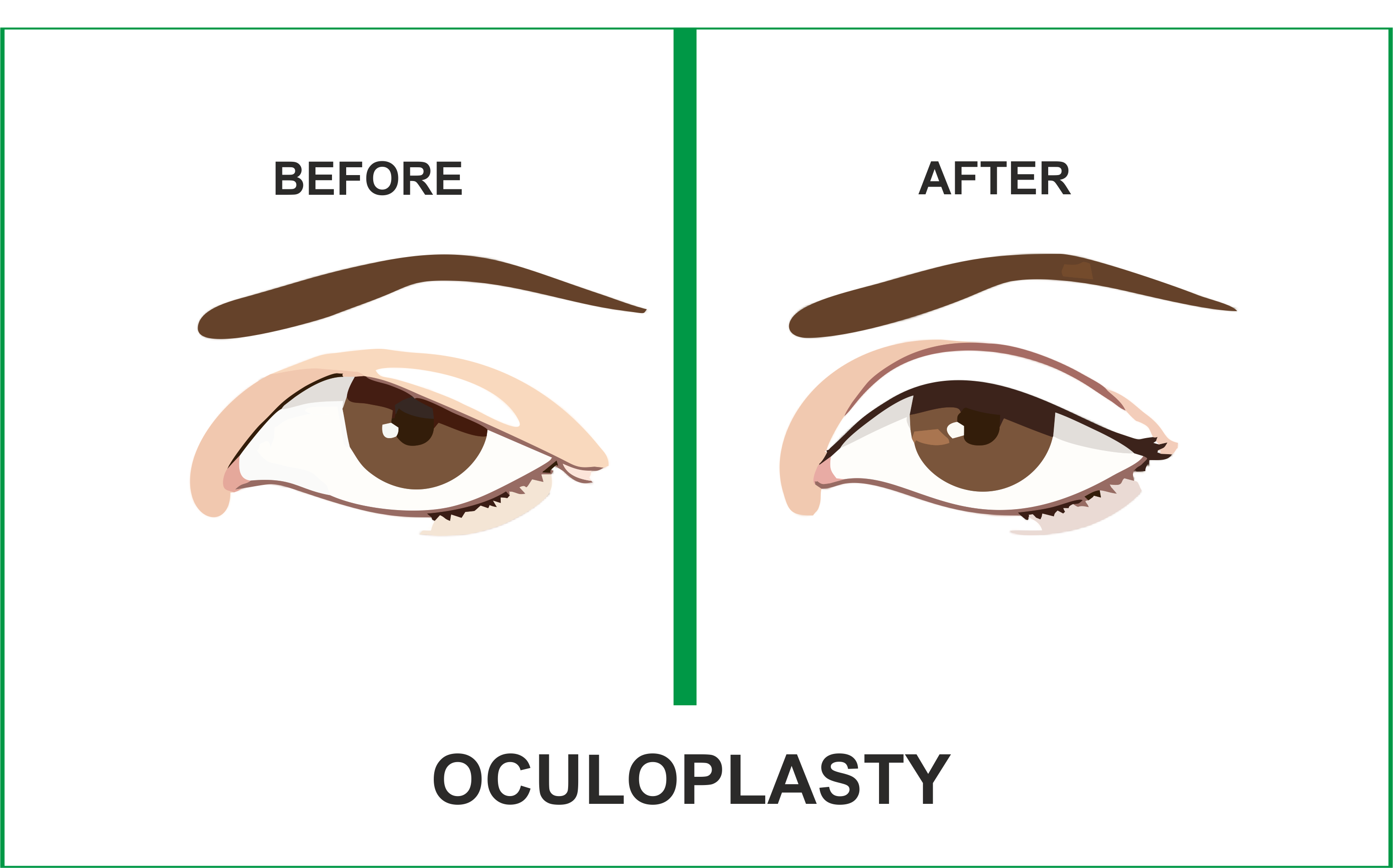
Preoperative Evaluation: The patient undergoes a comprehensive eye examination and consultation with an oculoplastic surgeon to assess the specific condition and determine the most appropriate treatment plan. This may include measurements of visual acuity, evaluation of eyelid position and function, imaging studies, and discussion of surgical goals and expectations.
Anesthesia: Before the surgery, the patient receives local or general anesthesia to numb the surgical area and ensure comfort during the procedure. The type of anesthesia used depends on the complexity of the surgery and the patient’s medical history and preferences.
Incision: Depending on the nature of the oculoplastic procedure, the surgeon makes small, carefully placed incisions in the skin or mucous membranes around the eyes or eyelids. These incisions are strategically located to minimize scarring and optimize surgical access.
Tissue Manipulation: Using specialized surgical instruments and techniques, the surgeon manipulates the tissues of the eyelids, orbit, or surrounding facial structures to achieve the desired outcome. This may involve removing excess tissue, repositioning muscles or tendons, or reconstructing damaged or deformed structures.
Closure: Once the surgical objectives are achieved, the surgeon carefully closes the incisions using fine sutures or tissue adhesives. Special attention is paid to achieving precise alignment and minimizing tension on the tissues to promote optimal healing and cosmetic outcomes.
Postoperative Care: After surgery, the patient is monitored closely in the recovery area to ensure stability and comfort. Antibiotic and anti-inflammatory medications may be prescribed to prevent infection and reduce swelling and discomfort. The patient receives instructions for postoperative care, including wound care, activity restrictions, and follow-up appointments.
Recovery: Recovery time varies depending on the complexity of the surgery and the individual’s healing process. Most patients experience some degree of swelling, bruising, and discomfort in the immediate postoperative period, which gradually resolves over time. Full recovery may take several weeks to months, during which patients are advised to avoid strenuous activities and protect the surgical area from trauma.
Corneal Transplant (Keratoplasty) surgery
Corneal Transplant (Keratoplasty) is the most common type of corneal surgery, involving the replacement of a damaged or diseased cornea with healthy donor tissue obtained from a deceased donor.
Here’s an overview of the Corneal Transplant (Keratoplasty) procedure:
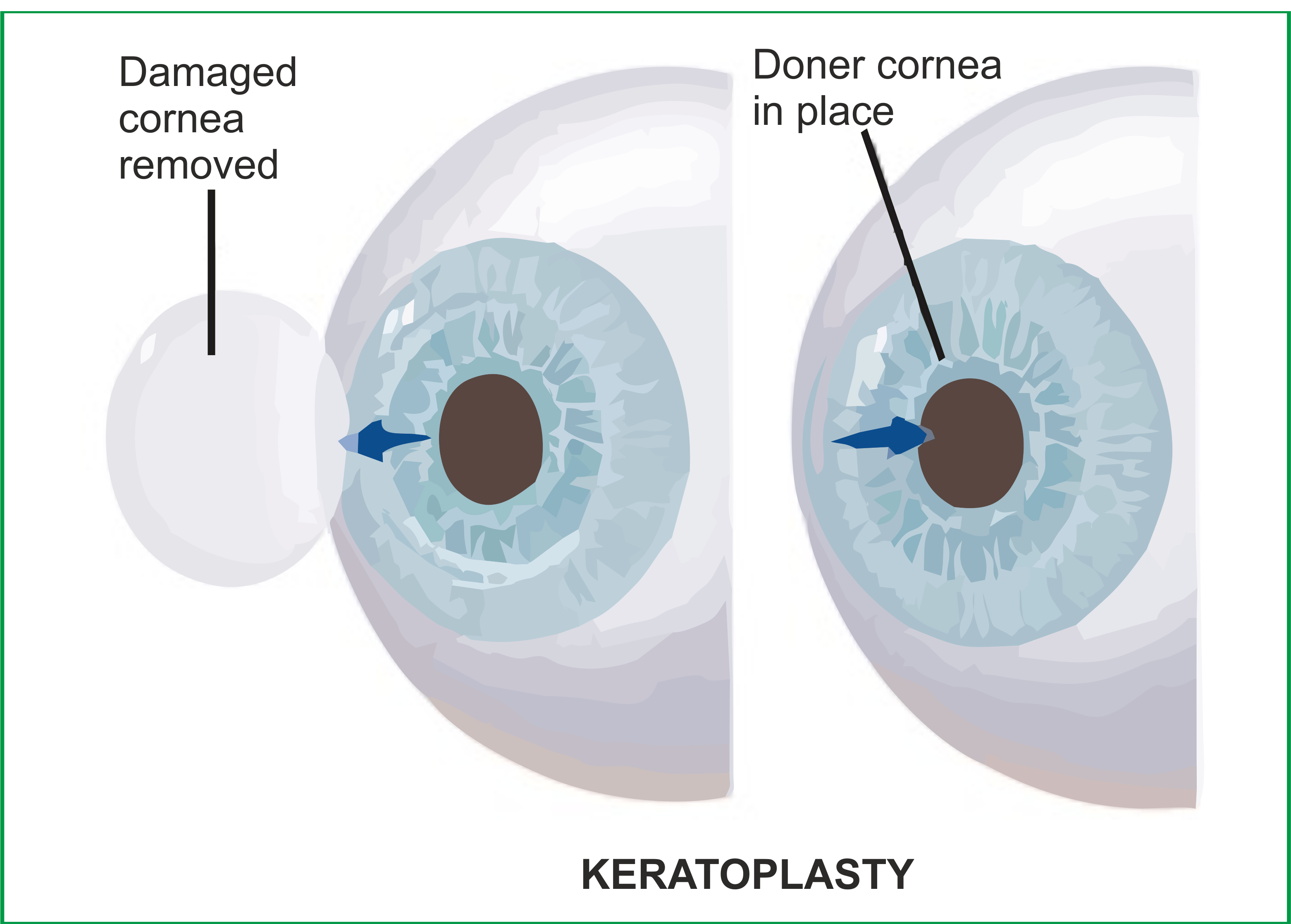
1) Preparation: Before the surgery, the patient undergoes a comprehensive eye examination to assess the health of the cornea and determine the need for transplantation. The patient’s medical history, including any previous eye surgeries or conditions, is reviewed. If a suitable donor cornea is available, arrangements are made for its procurement.
2) Anesthesia: The patient receives local or general anesthesia to numb the eye and surrounding tissues, ensuring comfort during the procedure.
3) Donor Cornea Preparation: If a deceased donor cornea is used for the transplant, it is carefully inspected and prepared in the operating room. The donor cornea is typically obtained from an eye bank and thoroughly evaluated to ensure its suitability for transplantation.
4) Recipient Cornea Preparation: The recipient’s eye is prepared for surgery by cleaning the surface of the cornea and marking the area where the transplant will be placed. In some cases, damaged or diseased corneal tissue may need to be removed before the transplant.
5) Graft Placement: Using microsurgical instruments, the surgeon carefully removes the central portion of the recipient’s cornea and replaces it with the donor cornea. The donor cornea is secured in place using sutures or an adhesive, ensuring proper alignment and stability.
6) Closure: Once the transplant is securely in place, the surgeon may close any incisions made in the eye using sutures or a self-sealing technique. The eye may be covered with a protective shield or bandage to promote healing and prevent infection.
7) Post-operative Care: After surgery, the patient is monitored closely in the recovery area to ensure stability and comfort. Antibiotic and anti-inflammatory eye drops may be prescribed to prevent infection and reduce inflammation. The patient receives instructions for post-operative care, including activity restrictions, medication regimens, and follow-up appointments.
8) Recovery: Recovery time varies depending on the complexity of the surgery and the individual’s healing process. Most patients experience improved vision over time, although full recovery may take several weeks to months. It’s important for patients to follow their surgeon’s instructions and attend all scheduled follow-up appointments to monitor healing and assess visual outcomes.
