Corneal Diseases
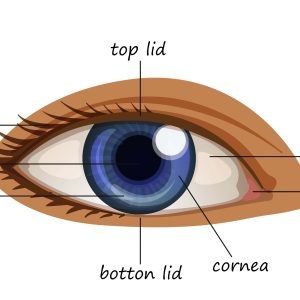
Corneal diseases encompass a range of conditions affecting the transparent front part of the eye, known as the cornea. This crucial component plays a vital role in focusing light and protecting the eye. Following is the list of some common Corneal Diseases.
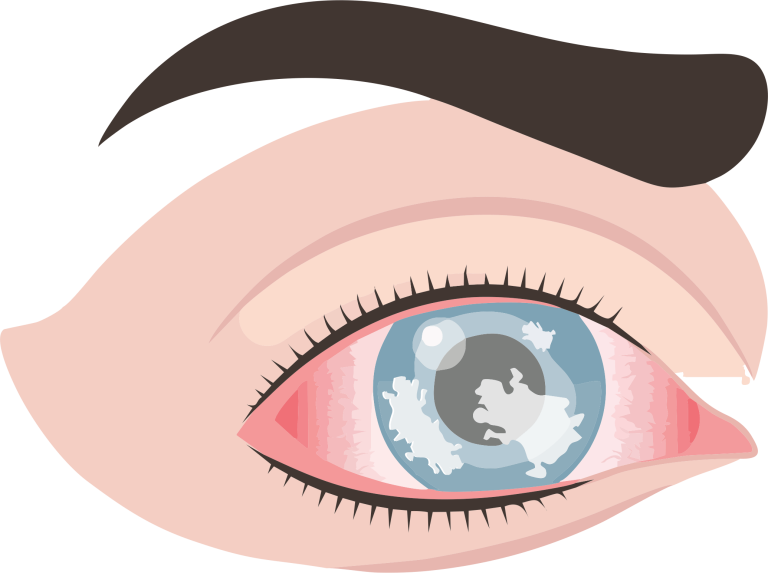
Keratitis is the inflammation of the cornea, the transparent front part of the eye covering the pupil and iris. It can be caused by various factors, leading to pain, blurred vision, and discomfort.
1. Infections: Bacterial, Viral, or fungal infections.
2. Injury: Scratches, cuts, or foreign objects in the eye.
3. Contact Lens Wear: Prolonged use or improper hygiene.
4. Dry Eyes: Insufficient tear production.
5. Underlying Conditions: Autoimmune diseases, like rheumatoid arthritis.
1. Eye Pain: Often severe and may worsen with blinking.
2. Redness: Bloodshot appearance of the eye.
3. Blurry Vision: Impaired or hazy vision.
4. Sensitivity to Light: Photophobia.
5. Excessive Tearing: Watery eyes.
6. Discharge: Pus or other discharge.
1. Bacterial Keratitis: Caused by bacterial infection.
2. Viral Keratitis: Caused by viruses like herpes simplex.
3. Fungal Keratitis: Caused by fungi, often in agricultural settings.
4. Acanthamoeba Keratitis: Rare, caused by amoeba found in water.